Botulism and Babies
Author: Ryan Sorkin, MD
Editor: Rahul Shah, MD
Case Presentation:
A ten week old boy is brought to the ED due to subjective fussiness and refusal to eat by his mother – their second visit for this concern. During their first ED visit, the patient improved with acetaminophen and IV fluids, and was able to be discharged home. Electrolytes were also obtained then, and were normal.
However, since being at home, mom reports that “he’s just not eating right.” Initially, mom had been exclusively breastfeeding, but has been trying to supplement with formula over the last few weeks due to poor intake.
Vital Signs:
HR: 155
RR: 42
SpO2 on RA: 99%
BP: 86/ 52
Physical Exam:
General: Tired-appearing and fussy, but easily consoled.
HEENT: Normocephalic. Mild rhinorrhea.
Cardiovascular: Heart rate normal for age. No murmur.
Abdomen: Soft, nontender, nondistended.
Neuro: Sluggish suck and mildly decreased tone in arms and neck.
Skin: He is well hydrated. He has mild rhinorrhea and some coarse breath sounds bilaterally.
The video above can be watched when viewed directly on YouTube. It contrasts normal and abnormal tone for a 2 month old – some findings may be subtle!
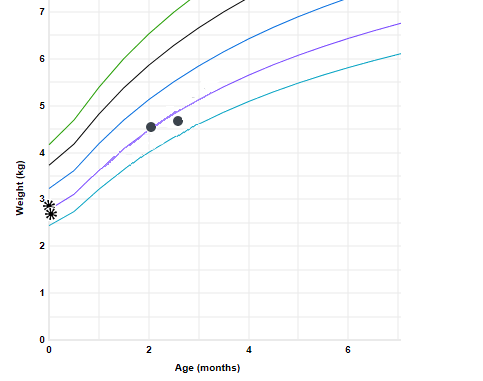
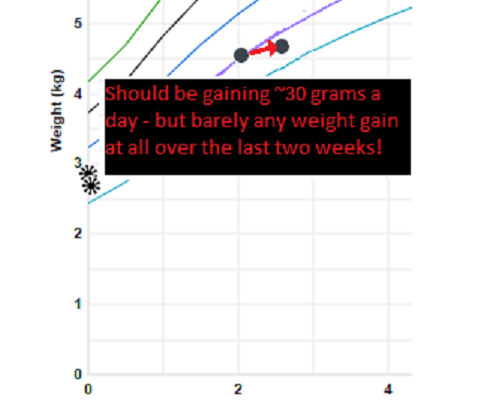
Always look at the growth chart!
At this point in life, our patient should be gaining 30 grams a day. This isn't happening.
Differential Diagnosis
Critical Clue
Presumed Diagnosis:
Objectives:
- What is the basic pathophysiology of foodborne botulism in infancy?
- What airway considerations should be made for this patient?
- How can I diagnose and treat botulism?

Discussion:
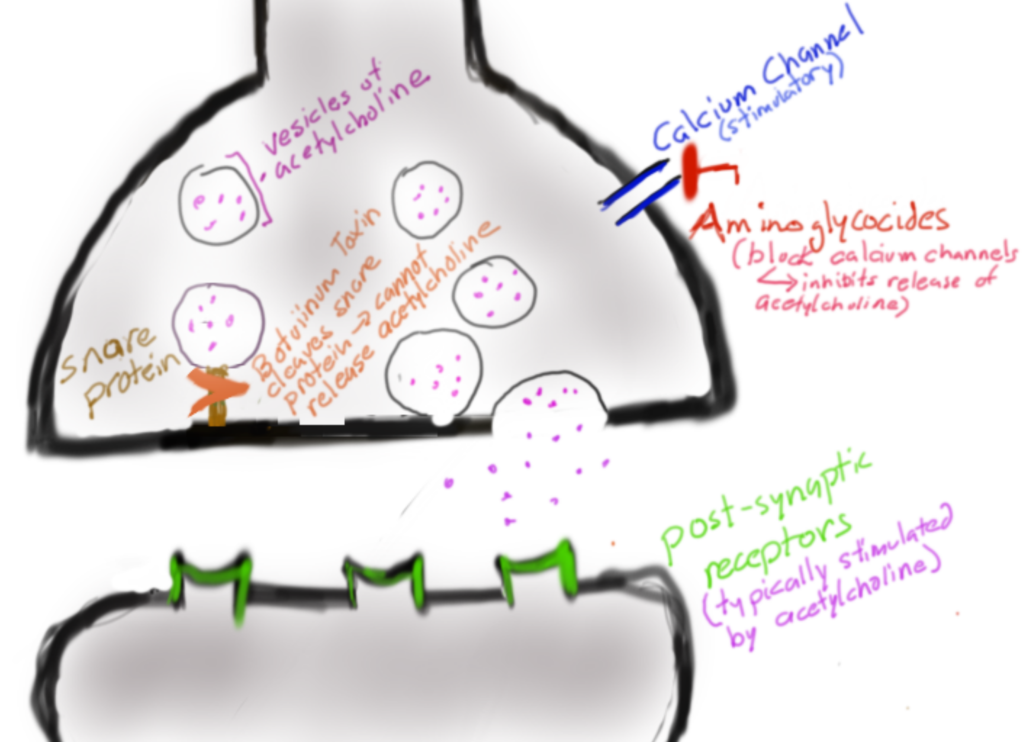
Infants have immature gut flora and a still-developing immune system. Given this, botulinum spores (which can be found in honey) may colonize the gut with Clostridium Botulinum. C. Botulinum produces botulism toxin, which upon entry to peripheral nerve cells, cleaves SNARE proteins. This means that vesicles with acetylcholine in the presynapatic cell cannot make it to cell membrane, which ultimately prevents the release of acetylcholine into the presynaptic cleft.
When older kids/ adults get botulism, it is typically due to ingestion of the preformed toxin, rather than the spores.
Botulism can be deadly because its toxin selectively targets motor neurons causing a form of paralysis. Some of the motor neurons that are essential to life are the ones that innervate the diaphragm and allow us to breathe. The toxin itself does not directly damage lungs, but they do prevent the ability to ventilate. Patients with suspected or confirmed botulism will need very close monitoring for respiratory failure. For progressive paralysis or impending respiratory failure, patients may need to be intubated to maintain ventilation while we attempt to treat the infection and manage symptoms.
This patient ultimately required intubation due to progressive respiratory failure while admitted.
A good exam can facilitate early diagnosis, but can be challenging. This patient had a weak suck and poor head control. In addition, the patient’s growth chart is worrisome. The following day, on the floor, the patient was found to have slow pupillary responses to light. The family was asked about consumption of honey products, which mom endorsed effectively clinching the diagnosis.
To confirm diagnosis you need to check stool for spores; serum is often negative in infantile botulism. Once diagnosis is confirmed, or botulism is strongly suspected, antitoxin should be given as soon as possible to bind circulating toxins. The antitoxin can only prevent further paralysis; that’s why early administration is so important.
Despite lengthy hospitalizations and necessary critical care for such patients, prognosis is very good. Symptoms improve once motor endplates and nerve terminals regenerate. Typically, diaphragmatic function is among the first to return.
Antibiotics should not be prescribed for infantile botulism as this can lead to a theoretical release of toxin.
Remember that botulism is a reportable disease! You must notify your state’s health department for any suspected cases.

1. Honey holds spores of Clostridium Botulinum which allow for intestinal colonization in infants – remember that infants (12 months old and less) should NOT consume honey. The resulting toxin inhibits acetylcholine release.
2. When botulism is suspected, monitor these patients for respiratory failure and be ready to intubate/ ventilate.
3. Consider botulism when you see poor tone and inadequate intake during infancy. Get antitoxin and confirmatory testing onboard immediately. Most hospitals do not carry botulism antitoxin; you need to contact the state health department to report any suspected cases and to get a dose.
Discussion Sources:
1.Wikström S, Holst E. Spädbarnsbotulism – skäl att inte ge honung till barn under ett år [Infant botulism – why honey should be avoided for children up to one year]. Lakartidningen. 2017 Jul 24;114:ELMF. Swedish. PMID: 28742188.
2. Rosow LK, Strober JB. Infant botulism: review and clinical update. Pediatr Neurol. 2015 May;52(5):487-92. doi: 10.1016/j.pediatrneurol.2015.01.006. Epub 2015 Jan 21. PMID: 25882077.
3. Hodowanec A, Bleck TP. Clostridium botulinum (Botulism). In: Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed, Bennett JE, Dolin R, Blaser MJ (Eds), Elsevier Saunders, Philadelphia 2015. p.2763.
4. Cox N, Hinkle R. Infant botulism. Am Fam Physician. 2002 Apr 1;65(7):1388-92. PMID: 11996423.
Muddiest Point: Why shouldn't I use antibiotics in treating botulism?
Some dated studies (from the 1970s) did not find any benefit with using pencillin-based antibiotics in treating botulism. Others found that aminoglycocides actually worsen some of the inhibitory neuromuscular effects from botulinium toxin by blocking calcium channels.
Moreover, there are several theoretical risks associated with antibiotic use. One argument suggests that when antibiotics kill bacterial cells, they would further release toxin in the bowel, leading to absorption. A second argument notes that all antibiotics affect intestinal bacteria by disturbing normal flora; the use of antibiotics may allow for unpredictable overgrowth of C. botulinum.
Muddiest Point Sources
- Brook, I. Infant botulism. J Perinatol 27, 175–180 (2007).
2. Lonati, Davide, Schicchi, Azzurra, Crevani, Marta, Buscaglia, Eleonora, Scaravaggi, Giulia, Maida, Francesca, Cirronis, Marco, Petrolini, Valeria Margherita, and Locatelli, Carlo Alessandro. “Foodborne Botulism: Clinical Diagnosis and Medical Treatment.” Toxins.12.8 (2020): 509. Web.
Have you seen a patient present similarly? Is there a different diagnosis you would consider? Do you have thoughts on the proposed management? Please leave any and all comments below!