Drooling Danger
Author: Charlie Lopez, MD
Editor: Rahul Shah, MD
Vital Signs:
Temp: 98F
HR: 102
RR: 25
SpO2 on RA: 100%
BP: 100/65
Physical Exam
General: well appearing infant, in no acute distress
HEENT: Atraumatic, PERRL, TM clear non-bulging without any foreign bodies, moist mucous membranes, mild drooling, no stridor
CV: heart RRR, no murmurs, cap refill < 2 sec
Chest: lungs clear bilateral
Abdomen: soft, non-tender
MSK: full ROM
Differential Diagnosis
Critical Clue
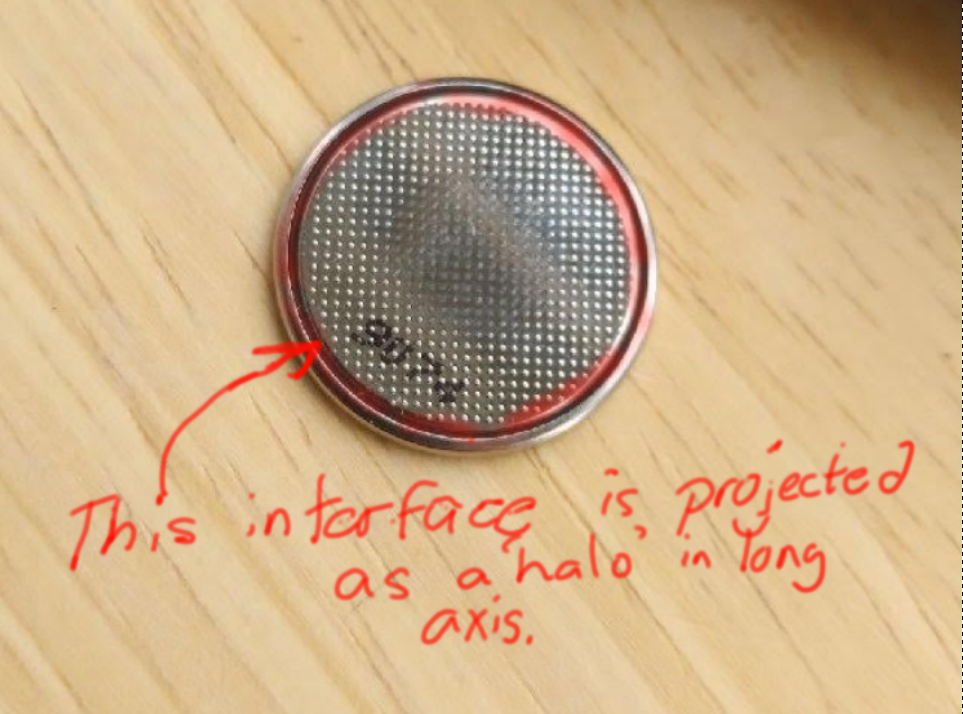
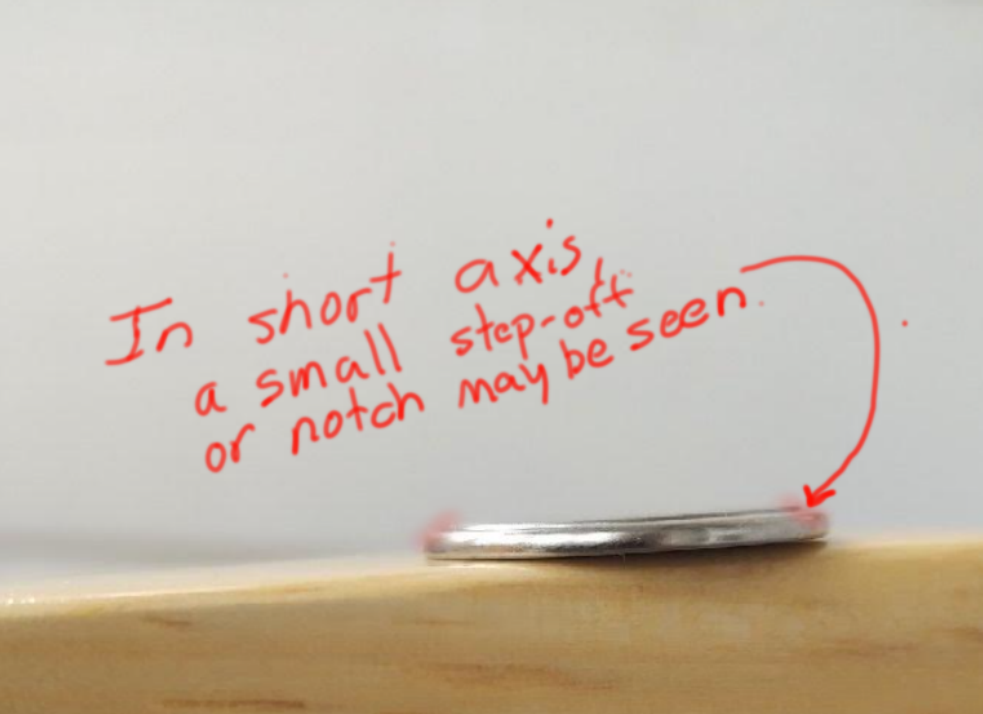
On the left, you see an AP Chest X-ray with a double ‘halo’ sign. This represents the notched interface between the negative and positive poles of the battery.
Objectives:
- Identify a potential foreign body ingestion
2. Recognize acuity of button battery ingestions sequelae
3. Determine appropriate management for button batter ingestions
In the case above, this child has had prior similar episodes with this non specific symptom. The key factor that lead to prompting further diagnostics was a change in character/severity of the symptoms. The father had reported new onset drooling and prolonged duration of symptoms.
A button battery ingestion may present subtly, especially if it was an unwitnessed event as in this case. Patients with these types of ingestions may be asymptomatic initially and may present with nonspecific symptoms to include dysphagia, nausea, vomiting, chest pain, drooling, difficulty breathing, and stridor.
The patient from this case looked well, but would have likely rapidly deteriorated if a high index of suspicion was not maintained.
After ingestion, the button battery comes in contact with the mucosa of the GI tract, causing hydrolysis and the formation of hydroxide solution, resulting in surrounding alkalinization and liquefactive necrosis.
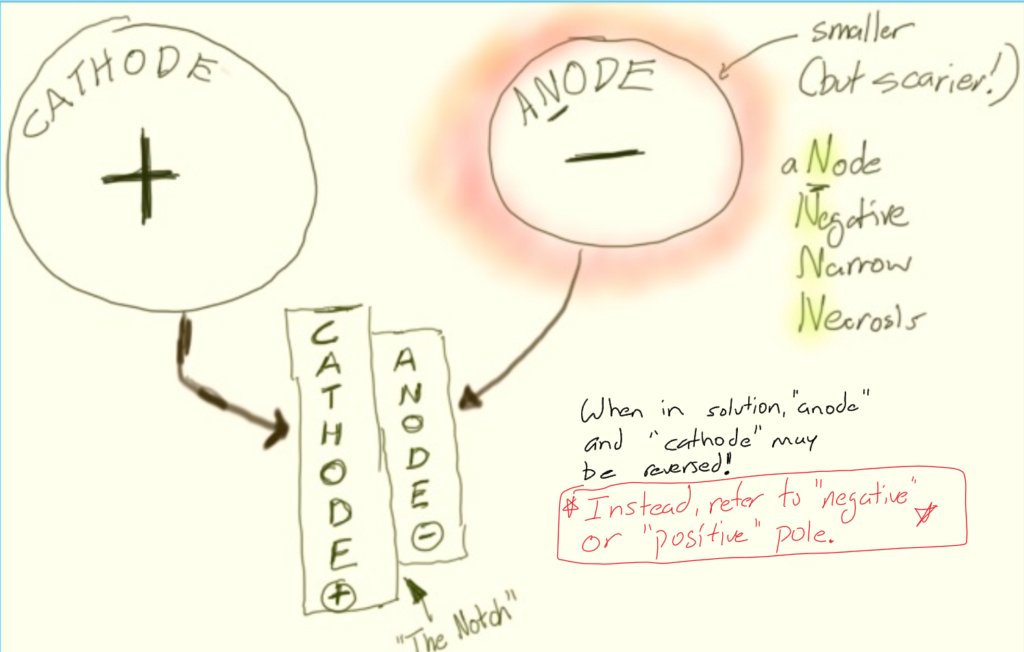
The negative pole (anode) of the button battery is the side where a reduction reaction takes place, leading to the accumulation of hydrogen gas and hydroxide ions . Often times this side is referred to as the anode, or the negative pole. However, often times when these batteries are immersed in solution, the poles can be redefined, depending where the reduction or oxidation process occurs. Thus, for the proposes of identifying the side of the battery where injury is likely to be worse, clinicians should refer to the site of reduction (site where hydroxide ions accumulate, as the negative pole. An anode facing anteriorly places a higher risk of formation of a tracheoesophageal fistula.
Complications of button battery ingestion include:
– Tracheoesophageal fistula
– Esophageal perforation
– Mediastinitis
– Vocal cord paralysis
– Tracheal stenosis
– Tracheomalacia
– Aspiration pneumonia
– Empyema
– Lung abscess
– Pneumothorax
– Spondylodiscitis
– Large vessel perforation and exsanguination
- As with any foreign body ingestion always ensure that the patient has a patent airway, breathing is not compromised, and circulation is intact. As there is potential for severe damage to mediastinal structures, be prepared to secure an emergent airway if needed.
- When suspected, immediate radiographic imaging should be obtained – Ideally an AP and lateral XR of neck, chest and abdomen. Or, if the patient is small enough, a single ‘babygram.’
- The main goal of esophageal button battery ingestion is endoscopic removal as soon as possible, ideally within 1 hour of presentation to the emergency department.
- Avoid inducing vomiting.
- Don’t try remove it blindly! Direct visualization of adjacent tissues is needed to assess the extent of injuries
- Patients should be NPO for OR, however consider honey or Carafate (see below) depending on your anticipated time to removal.
- The administration of honey (if >12 mo) or Carafate has been shown to reduce the severity of injury from button battery ingestion both in vitro and in vivo, and should be strongly considered..
- Anticipate admission to the ICU for these patients for careful monitoring and potential for serial endoscopy and/or bronchoscopy.
A Team Approach is the Best Approach
Time to removal in the OR, thus limiting tissue damage and further morbidity and mortality must be optimized. The triage of these patients can significantly impact time to OR. Having a coordinated response to suspected button battery ingestion is crucial in improving patient outcomes. It has been shown that if such a patient was triaged as a trauma activation, thus having OR staff prepared, has been shown to decrease the amount of time from presentation to the OR. Ideally, an anesthesiologist proficient with pediatrics should be present for such activations as well. In situations where all of the resources afforded to a level 1 center are not available, timely transfer to an appropriate facility must be done. In such a circumstance, the physician must discuss and weight the risks and benefit of delayed removal after transfer vs removal at present facility.

- Always consider foreign body ingestion for infants and toddlers who present with drooling, vomiting abdominal pain and/or respiratory complaints.
- Time is tissue! The longer a button battery remains in the body the more potential for significant tissue damage
- If the situation allows, remember treatments that can be used to reduce severity of injury to include honey (only if at least 12 months old!) and Carafate.
Discussion Sources:
- Button Battery Ingestion: A True Surgical and Anesthetic Emergency Templeton, T. Wesley M.D.; Terry, Bradley J. M.D.; Pecorella, Shelly H. M.D.; Downard, Martina G. M.D.
- Anfang, Rachel R, Jatana, Kris R, Linn, Rebecca L, Rhoades, Keith, Fry, Jared, and Jacobs, Ian N. “PH‐neutralizing Esophageal Irrigations as a Novel Mitigation Strategy for Button Battery Injury.” The Laryngoscope1 (2019): 49-57. Web.
- Ing, R.J., Hoagland, M., Mayes, L. et al.The anesthetic management of button battery ingestion in children. Can J Anesth/J Can Anesth 65, 309–318 (2018). https://doi-org.online.uchc.edu/10.1007/s12630-017-1023-9
- Russell, Robert T, Griffin, Russell L, Weinstein, Elizabeth, and Billmire, Deborah F. “Esophageal Button Battery Ingestions: Decreasing Time to Operative Intervention by Level I Trauma Activation.” Journal of Pediatric Surgery9 (2014): 1360-362. Web.
- https://www.poison.org/battery
Muddiest Point: Why are foreign bodies seen in short axis on an AP film more likely to be in the trachea rather than the esophagus?
Answer: They aren’t. classic teaching suggests that with a standard AP film, a button battery is in the esophagus when it is seen in long-axis, and in the trachea when seen in short-axis. However, this does not appear to be backed by evidence. In fact, irrespective of its orientation on your film, it is most likely in the esophagus.
Ultimately, foreign bodies are far more likely to wind up in the esophagus rather than the trachea. However, if you catch one in a sagittal plane (short axis) on an AP/PA film, shoot a lateral. Remember that the trachea is anterior to the esophagus, and you should be able to decipher where the foreign body is!
Muddiest Point Sources
1. Schlesinger AE, Crowe JE. Sagittal orientation of ingested coins in the esophagus in children. AJR Am J Roentgenol. 2011 Mar;196(3):670-2. doi: 10.2214/AJR.10.5386. PMID: 21343512
2.Raney LH, Losek JD. Child with esophageal coin and atypical radiograph. J Emerg Med. 2008 Jan;34(1):63-6. doi: 10.1016/j.jemermed.2007.03.004. Epub 2007 Jul 20. PMID: 17976776.
Have you seen a patient present similarly? Is there a different diagnosis you would consider? Do you have thoughts on the proposed management? Please leave any and all comments below!